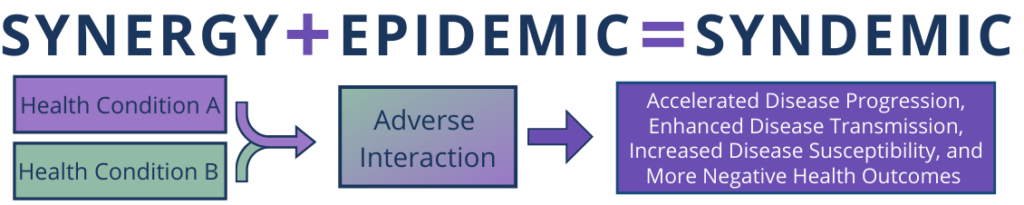
The word syndemic comes from two more commonly understood terms: synergy and epidemic. Synergy: the interaction of two or more agents that produces a combined effect greater than the sum of their separate efforts. Epidemic: the widespread occurrence of a health condition in a community at a particular time. Syndemic: two or more overlapping epidemics connected through behavior, biology, and social conditions resulting in enhanced health burden across a population.
To be considered a syndemic three criteria need to be met: (1) data demonstrate separate epidemics are occurring; (2) health conditions interact through behavior or biology to increase overall health burden; and (3) systems-level factors contribute to and sustain the epidemics.

The health areas included in the Tennessee End the Syndemic initiative are: human immunodeficiency virus (HIV), sexually transmitted infections (STIs), substance use disorder (SUD), and viral hepatitis (VH).

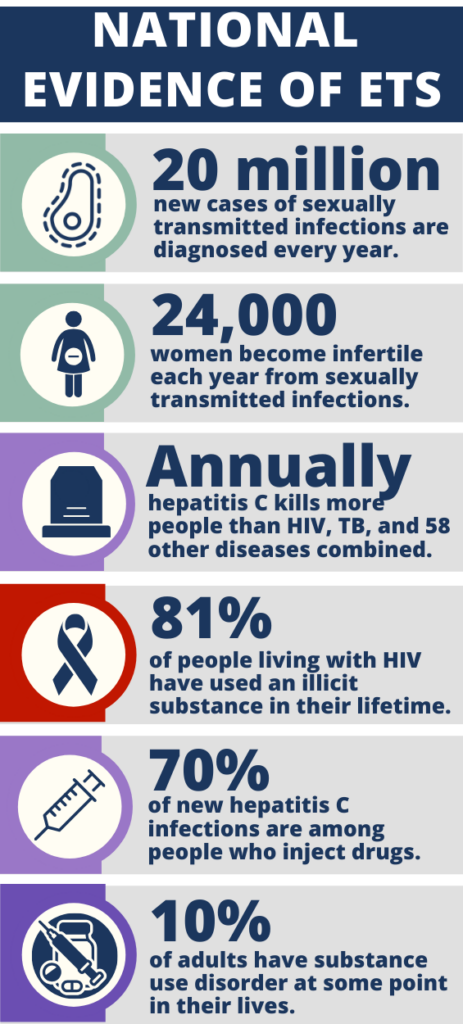
Sexually transmitted infections (STIs) reached an all-time high in 2018, with 20 million new cases each year. (1). Between 2014 and 2018, chlamydia cases have increased by 19%, gonorrhea by 63%, primary and secondary syphilis by 71%, and congenital syphilis by 185% (2). Annually, 24,000 women become infertile as a result of untreated STIs (3). Viral hepatitis has also seen notable shifts in the number of annual cases. With large hepatitis A outbreaks sweeping the nation, the hepatitis A rate of infection nearly doubled between 2013 and 2017, from 0.6 to 1.0 cases per 100,000 people (4). Despite being vaccine preventable and a routine childhood vaccination, new hepatitis B infections continue to persist. Cases of hepatitis C cases have been trending upward nationwide since 2013 (4). Hepatitis C infections that are left untreated can be deadly. Since 2013, hepatitis C has killed more Americans annually than HIV, tuberculosis, and 58 other reportable infectious diseases combined (5).
According to National Institutes of health, approximately 10% of U.S. adults have drug disorder at some point in their lives and 75% report never receiving any form of treatment (6). Substance use is common among people living with HIV (PLWH) with nearly 50% of PLWH reporting current or past histories of drug or alcohol disorders (7). Nationally, up to 70% of new hepatitis C infections are among people who inject drugs (8). Men who have sex with other men, transgender persons, young adults, and some racial and ethnic groups, including Black and Latinx, are disproportionately affected by many of these health conditions.
According to National Institutes of health, approximately 10% of U.S. adults have drug disorder at some point in their lives and 75% report never receiving any form of treatment (6). Substance use is common among people living with HIV (PLWH) with nearly 50% of PLWH reporting current or past histories of drug or alcohol disorders (7). Nationally, up to 70% of new hepatitis C infections are among people who inject drugs (8). Men who have sex with other men, transgender persons, young adults, and some racial and ethnic groups, including Black and Latinx, are disproportionately affected by many of these health conditions.
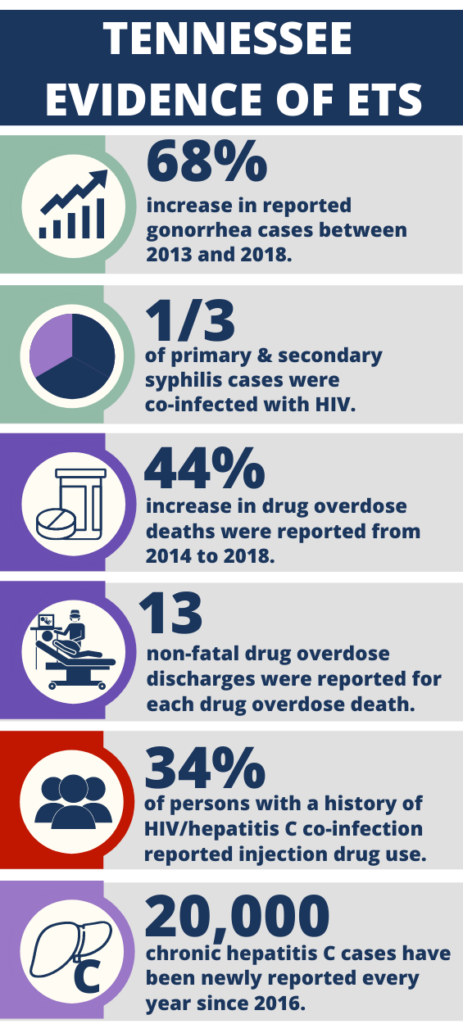
Despite national decreases, Tennessee observed a 44% increase in drug overdose deaths from 2014 to 2018. For every life lost to drug overdose in 2018, 13 people were discharged from Tennessee hospitals for non-fatal drug overdoses. As substance use continues to increase, so does the concern of a rapid transmission event of HIV and hepatitis C due to Injection drug use. Approximately 34% of people living with HIV with a history of hepatitis C infection, report injection drug use. Since 2016, there have been 20,000 newly reported cases of chronic hepatitis C each year.
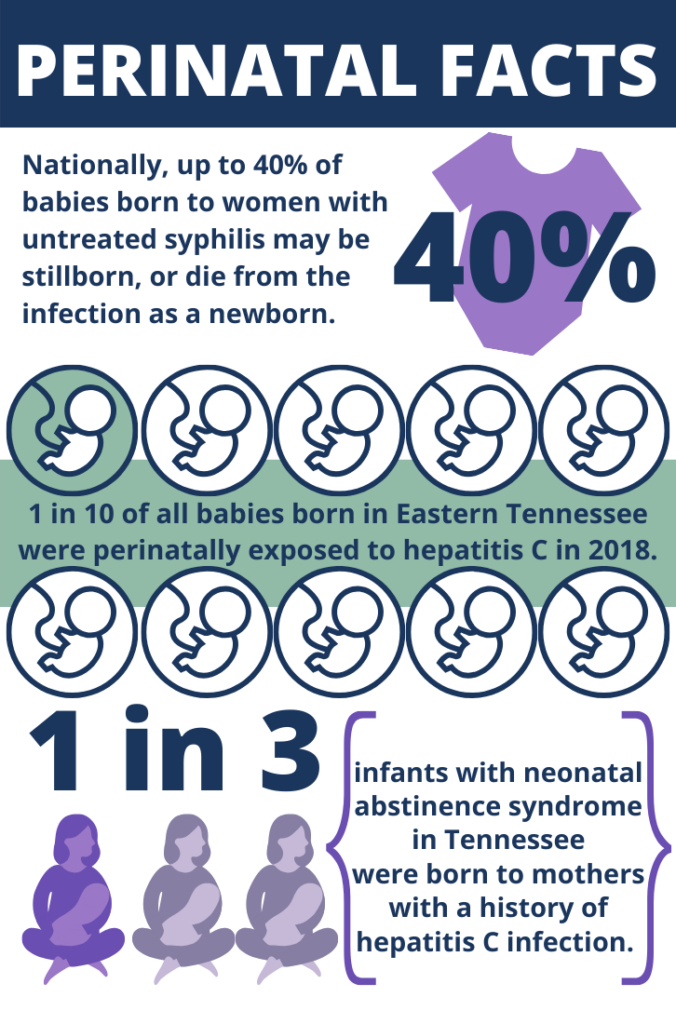
Nationally, 40% of babies born to women with untreated syphilis will be stillborn or die from the infection as a newborn and over the last few years Tennessee has seen a notable increase in congential syphilis cases. As the distribution of hepatitis C cases continues to shift toward younger individuals, concerns about the impact of hepatitis C virus infection among reproductive-aged women and potential transmission of the virus to their infant(s) grows.In eastern Tennesee, approximately 10% of all babies born were exposed perinatally to hepatitis C in 2018. The crossover between hepatitis C and substance use emerges clearly in the number of infants born with neonatal abstience syndrome (NAS). Approximately one third of infants with NAS were born to mothers with a history of hepatitis C infection. As we move to end the syndemic in Tennesee, addressing the unqiue needs pregnant persons and their infants will be critical to ending the sydnemic for future generations

The data dashboards listed below are interactive tools that contain the most up-to-date state, regional, and county level data on drug overdoses, mental health and substance abuse services, and HIV trends. The HIV and Hepatitis C Virus (HCV) Outbreak Vulnerability Dashboard contains profiles for each county in Tennessee about their vulnerability to an HIV or HCV rapid transmission event due to injection drug use.
Below are the most recent epidemiological profiles where in-depth data and analysis can be found on the various health topics included in the syndemic.
1.https://www.cdc.gov/std/dstdp/2018-SR-DCL_FINAL.pdf
2.https://www.cdc.gov/std/stats18/default.htm
3.https://www.cdc.gov/std/health-disparities/stds-women-042011.pdf
4.https://www.cdc.gov/hepatitis/statistics/2017surveillance/index.htm
5.https://www.cdc.gov/media/releases/2016/p0504-hepc-mortality.html
© 2022 End The Syndemic TN. All rights reserved.